Empower Your Audiobook Journey
4 Steps to Master the Art of Mindful Speaking
By Andreas Berkey
Illustrations by Madelyn Neufeld
Copyright © 2024 by Andreas Berkey
References by Chapter
Chapter 1:
Acevedo, B. P., Aron, A., Fisher, H. E., & Brown, L. L. (2012). Neural correlates of long-term intense romantic love. Social cognitive and affective neuroscience, 7(2), 145–159. Neural correlates of long-term intense romantic love
Gupta, R., Koscik, T. R., Bechara, A., & Tranel, D. (2011). The amygdala and decision-making. Neuropsychologia, 49(4), 760–766. https://doi.org/10.1016/j.neuropsychologia.2010.09.029
Teles R. V. (2020). Phineas Gage’s great legacy. Dementia & neuropsychologia, 14(4), 419–421. Phineas Gage's great legacy
Van Horn, J. D., Irimia, A., Torgerson, C. M., Chambers, M. C., Kikinis, R., & Toga, A. W. (2012). Mapping connectivity damage in the case of Phineas Gage. PloS one, 7(5), e37454. Mapping Connectivity Damage in the Case of Phineas Gage
Chapter 2:
Byrne, E. (2017). Swearing is go*d f*r you: the amaz!ng sc!ence of bad language. Profile Books.
Hansen SJ, McMahon KL, de Zubicaray GI. The neurobiology of taboo language processing: fMRI evidence during spoken word production. Soc Cogn Affect Neurosci. 2019 Mar 5;14(3):271-279. doi: 10.1093/scan/nsz009. PMID: 30715549; PMCID: PMC6399611.
Teles R. V. (2020). Phineas Gage’s great legacy. Dementia & neuropsychologia, 14(4), 419–421. Phineas Gage's great legacy
Van Horn, J. D., Irimia, A., Torgerson, C. M., Chambers, M. C., Kikinis, R., & Toga, A. W. (2012). Mapping connectivity damage in the case of Phineas Gage. PloS one, 7(5), e37454. Mapping Connectivity Damage in the Case of Phineas Gage
Chapter 4:
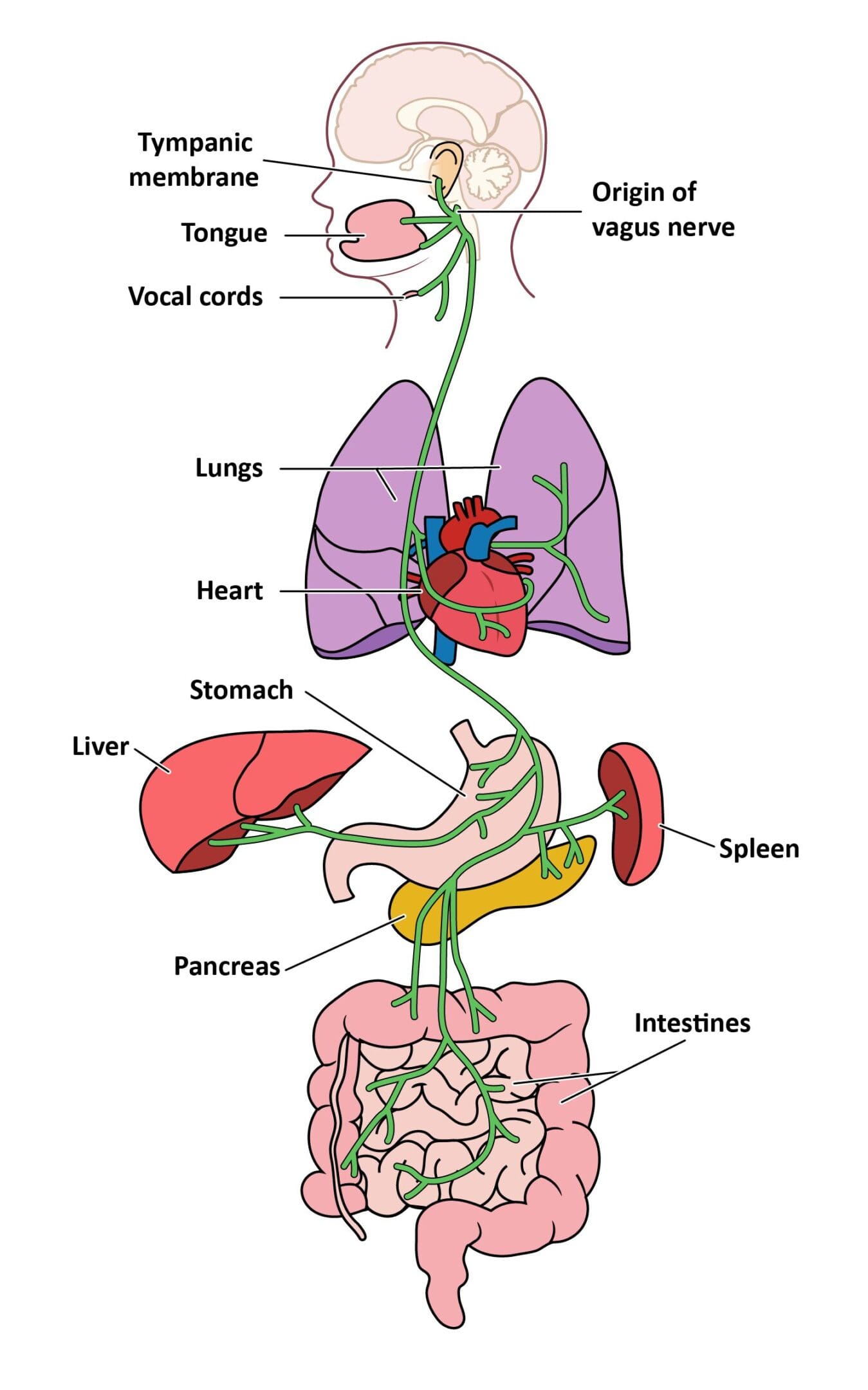
Bonaz, B., Bazin, T., & Pellissier, S. (2018). The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis. Frontiers in Neuroscience, 12(49). Frontiers | The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis
Breit, S., Kupferberg, A., Rogler, G., & Hasler, G. (2018). Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders. Frontiers in Psychiatry, 9(44). Frontiers | Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders
Chakrabarti, A., Geurts, L., Hoyles, L., Iozzo, P., Kraneveld, A. D., La Fata, G., Miani, M., Patterson, E., Pot, B., Shortt, C., & Vauzour, D. (2022). The microbiota–gut–brain axis: pathways to better brain health. Perspectives on what we know, what we need to investigate and how to put knowledge into practice. Cellular and Molecular Life Sciences, 79(2). The microbiota–gut–brain axis: pathways to better brain health. Perspectives on what we know, what we need to investigate and how to put knowledge into practice
De Couck, M., Caers, R., Musch, L., Fliegauf, J., Giangreco, A., & Gidron, Y. (2019). How breathing can help you make better decisions: Two studies on the effects of breathing patterns on heart rate variability and decision-making in business cases. International Journal of Psychophysiology, 139, 1–9. https://doi.org/10.1016/j.ijpsycho.2019.02.011
Diener, C., Dai, C. L., Wilmanski, T., Baloni, P., Smith, B., Rappaport, N., Hood, L., Magis, A. T., & Gibbons, S. M. (2022). Genome–microbiome interplay provides insight into the determinants of the human blood metabolome. Nature Metabolism, 4(11), 1560–1572. Genome–microbiome interplay provides insight into the determinants of the human blood metabolome
Góralczyk-Binkowska, A., Szmajda-Krygier, D. &_Kozlowska, E. 2022). The Microbiota–Gut–Brain Axis in Psychiatric Disorders. International Journal of Molecular Sciences, 23(19), 11245. The Microbiota–Gut–Brain Axis in Psychiatric Disorders
Magnon, V., Dutheil, F., & Vallet, G. T. (2021). Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults. Scientific Reports, 11(1). Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults
Mayer, E. A., Nance, K., & Chen, S. (2022). The Gut–Brain Axis. Annual Review of Medicine, 73(1), 439–453. The Gut–Brain Axis
Shi, L., Ju, P., Meng, X., Wang, Z., Yao, L., Zheng, M., Cheng, X., Li, J., Yu, T., Xia, Q., Yan, J., Zhu, C., & Zhang, X. (2023). Intricate role of intestinal microbe and metabolite in schizophrenia. BMC Psychiatry, 23(1). Intricate role of intestinal microbe and metabolite in schizophrenia - BMC Psychiatry
Socala, K., Doboszewska, U., Szopa, A., Serefko, A., Wlodarczyk, M., Zielinska, A., Poleszak, E., Fichna, J. & Wlaz, P. (2021). The role of microbiota-gut-brain axis in neuropsychiatric and neurological disorders. Pharmacological Research, 172, 105840. https://doi.org/10.1016/j.phrs.2021.105840
Van Treuren, W., & Dodd, D. (2017). Microbial Contribution to the Human Metabolome: Implications for Health and Disease. Annual Review of Pathology: Mechanisms of Disease, 15(1). Microbial Contribution to the Human Metabolome: Implications for Health and Disease
Zhu, F., Guo, R., Wang, W., Ju, Y., Wang, Q., Ma, Q., Sun, Q., Fan, Y., Xie, Y., Yang, Z., Jie, Z., Zhao, B., Xiao, L., Yang, L., Zhang, T., Liu, B., Guo, L., He, X., Chen, Y., & Chen, C. (2019). Transplantation of microbiota from drug-free patients with schizophrenia causes schizophrenia-like abnormal behaviors and dysregulated kynurenine metabolism in mice. Molecular Psychiatry. Transplantation of microbiota from drug-free patients with schizophrenia causes schizophrenia-like abnormal behaviors and dysregulated kynurenine metabolism in mice
Chapter Three:
Chapter 11:
Alfredsson, L., Armstrong, B. K., Butterfield, D. A., Chowdhury, R., de Gruijl, F. R., Feelisch, M., Garland, C. F., Hart, P. H., Hoel, D. G., Jacobsen, R., Lindqvist, P. G., Llewellyn, D. J., Tiemeier, H., Weller, R. B., & Young, A. R. (2020). Insufficient Sun Exposure Has Become a Real Public Health Problem.
International journal of environmental research and public health, 17(14), 5014. Insufficient Sun Exposure Has Become a Real Public Health Problem
Barbería-Latasa, M., Gea, A., & Martínez-González, M. A. (2022). Alcohol, Drinking Pattern, and Chronic Disease. Nutrients, 14(9), 1954. Alcohol, Drinking Pattern, and Chronic Disease
Barrett, L. F., & Simmons, W. K. (2015). Interoceptive predictions in the brain. Nature reviews. Neuroscience, 16(7), 419–429. Interoceptive predictions in the brain
Gad, I., Tan, X. C., Williams, S., Itawi, S., Dahbour, L., Rotter, Z., Mitro, G., Rusch, C., Perkins, S., & Ali, I. (2022). The Religious and Spiritual Needs of Patients in the Hospital Setting Do Not Depend on Patient Level of Religious/Spiritual Observance and Should be Initiated by Healthcare Providers. Journal of religion and health, 61(2), 1120–1138. The Religious and Spiritual Needs of Patients in the Hospital Setting Do Not Depend on Patient Level of Religious/Spiritual Observance and Should be Initiated by Healthcare Providers
Giménez, M. C., Hessels, M., van de Werken, M., de Vries, B., Beersma, D. G., & Gordijn, M. C. (2010). Effects of artificial dawn on subjective ratings of sleep inertia and dim light melatonin onset. Chronobiology international, 27(6), 1219–1241. https://doi.org/10.3109/07420528.2010.496912
Irwin M. R. (2019). Sleep and inflammation: partners in sickness and in health. Nature reviews. Immunology, 19(11), 702–715. Sleep and inflammation: partners in sickness and in health
Kang, J., Scholp, A., & Jiang, J. J. (2018). A Review of the Physiological Effects and Mechanisms of Singing. Journal of voice: official journal of the Voice Foundation, 32(4), 390–395. A Review of the Physiological Effects and Mechanisms of Singing
Puchalski, C. M., King, S. D. W., & Ferrell, B. R. (2018). Spiritual Considerations. Hematology/oncology clinics of North America, 32(3), 505–517. https://doi.org/10.1016/j.hoc.2018.01.011
Tamplin, J., Baker, F. A., Grocke, D., Brazzale, D. J., Pretto, J. J., Ruehland, W. R., Buttifant, M., Brown, D. J., & Berlowitz, D. J. (2013). Effect of singing on respiratory function, voice, and mood after quadriplegia: a randomized controlled trial. Archives of physical medicine and rehabilitation, 94(3), 426–434. Effect of Singing on Respiratory Function, Voice, and Mood After Quadriplegia: A Randomized Controlled Trial
Willemse, S., Smeets, W., van Leeuwen, E., Nielen-Rosier, T., Janssen, L., & Foudraine, N. (2020). Spiritual care in the intensive care unit: An integrative literature research. Journal of critical care, 57, 55–78. https://doi.org/10.1016/j.jcrc.2020.01.026
Zielinski, M. R., & Gibbons, A. J. (2022). Neuroinflammation, Sleep, and Circadian Rhythms. Frontiers in cellular and infection microbiology, 12, 853096. Frontiers | Neuroinflammation, Sleep, and Circadian Rhythms
Chapter 1:
Acevedo, B. P., Aron, A., Fisher, H. E., & Brown, L. L. (2012). Neural correlates of long-term intense romantic love. Social cognitive and affective neuroscience, 7(2), 145–159. Neural correlates of long-term intense romantic love
Gupta, R., Koscik, T. R., Bechara, A., & Tranel, D. (2011). The amygdala and decision-making. Neuropsychologia, 49(4), 760–766. https://doi.org/10.1016/j.neuropsychologia.2010.09.029
Teles R. V. (2020). Phineas Gage’s great legacy. Dementia & neuropsychologia, 14(4), 419–421. Phineas Gage's great legacy
Van Horn, J. D., Irimia, A., Torgerson, C. M., Chambers, M. C., Kikinis, R., & Toga, A. W. (2012). Mapping connectivity damage in the case of Phineas Gage. PloS one, 7(5), e37454. Mapping Connectivity Damage in the Case of Phineas Gage
Chapter 2:
Byrne, E. (2017). Swearing is go*d f*r you: the amaz!ng sc!ence of bad language. Profile Books.
Hansen SJ, McMahon KL, de Zubicaray GI. The neurobiology of taboo language processing: fMRI evidence during spoken word production. Soc Cogn Affect Neurosci. 2019 Mar 5;14(3):271-279. doi: 10.1093/scan/nsz009. PMID: 30715549; PMCID: PMC6399611.
Teles R. V. (2020). Phineas Gage’s great legacy. Dementia & neuropsychologia, 14(4), 419–421. Phineas Gage's great legacy
Van Horn, J. D., Irimia, A., Torgerson, C. M., Chambers, M. C., Kikinis, R., & Toga, A. W. (2012). Mapping connectivity damage in the case of Phineas Gage. PloS one, 7(5), e37454. Mapping Connectivity Damage in the Case of Phineas Gage
Chapter Three:
Chapter 4:
Bonaz, B., Bazin, T., & Pellissier, S. (2018). The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis. Frontiers in Neuroscience, 12(49). Frontiers | The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis
Breit, S., Kupferberg, A., Rogler, G., & Hasler, G. (2018). Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders. Frontiers in Psychiatry, 9(44). Frontiers | Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders
Chakrabarti, A., Geurts, L., Hoyles, L., Iozzo, P., Kraneveld, A. D., La Fata, G., Miani, M., Patterson, E., Pot, B., Shortt, C., & Vauzour, D. (2022). The microbiota–gut–brain axis: pathways to better brain health. Perspectives on what we know, what we need to investigate and how to put knowledge into practice. Cellular and Molecular Life Sciences, 79(2). The microbiota–gut–brain axis: pathways to better brain health. Perspectives on what we know, what we need to investigate and how to put knowledge into practice
De Couck, M., Caers, R., Musch, L., Fliegauf, J., Giangreco, A., & Gidron, Y. (2019). How breathing can help you make better decisions: Two studies on the effects of breathing patterns on heart rate variability and decision-making in business cases. International Journal of Psychophysiology, 139, 1–9. https://doi.org/10.1016/j.ijpsycho.2019.02.011
Diener, C., Dai, C. L., Wilmanski, T., Baloni, P., Smith, B., Rappaport, N., Hood, L., Magis, A. T., & Gibbons, S. M. (2022). Genome–microbiome interplay provides insight into the determinants of the human blood metabolome. Nature Metabolism, 4(11), 1560–1572. Genome–microbiome interplay provides insight into the determinants of the human blood metabolome
Góralczyk-Binkowska, A., Szmajda-Krygier, D. &_Kozlowska, E. 2022). The Microbiota–Gut–Brain Axis in Psychiatric Disorders. International Journal of Molecular Sciences, 23(19), 11245. The Microbiota–Gut–Brain Axis in Psychiatric Disorders
Magnon, V., Dutheil, F., & Vallet, G. T. (2021). Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults. Scientific Reports, 11(1). Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults
Mayer, E. A., Nance, K., & Chen, S. (2022). The Gut–Brain Axis. Annual Review of Medicine, 73(1), 439–453. The Gut–Brain Axis
Shi, L., Ju, P., Meng, X., Wang, Z., Yao, L., Zheng, M., Cheng, X., Li, J., Yu, T., Xia, Q., Yan, J., Zhu, C., & Zhang, X. (2023). Intricate role of intestinal microbe and metabolite in schizophrenia. BMC Psychiatry, 23(1). Intricate role of intestinal microbe and metabolite in schizophrenia - BMC Psychiatry
Socala, K., Doboszewska, U., Szopa, A., Serefko, A., Wlodarczyk, M., Zielinska, A., Poleszak, E., Fichna, J. & Wlaz, P. (2021). The role of microbiota-gut-brain axis in neuropsychiatric and neurological disorders. Pharmacological Research, 172, 105840. https://doi.org/10.1016/j.phrs.2021.105840
Van Treuren, W., & Dodd, D. (2017). Microbial Contribution to the Human Metabolome: Implications for Health and Disease. Annual Review of Pathology: Mechanisms of Disease, 15(1). Microbial Contribution to the Human Metabolome: Implications for Health and Disease
Zhu, F., Guo, R., Wang, W., Ju, Y., Wang, Q., Ma, Q., Sun, Q., Fan, Y., Xie, Y., Yang, Z., Jie, Z., Zhao, B., Xiao, L., Yang, L., Zhang, T., Liu, B., Guo, L., He, X., Chen, Y., & Chen, C. (2019). Transplantation of microbiota from drug-free patients with schizophrenia causes schizophrenia-like abnormal behaviors and dysregulated kynurenine metabolism in mice. Molecular Psychiatry. Transplantation of microbiota from drug-free patients with schizophrenia causes schizophrenia-like abnormal behaviors and dysregulated kynurenine metabolism in mice
Chapter 11:
Alfredsson, L., Armstrong, B. K., Butterfield, D. A., Chowdhury, R., de Gruijl, F. R., Feelisch, M., Garland, C. F., Hart, P. H., Hoel, D. G., Jacobsen, R., Lindqvist, P. G., Llewellyn, D. J., Tiemeier, H., Weller, R. B., & Young, A. R. (2020). Insufficient Sun Exposure Has Become a Real Public Health Problem.
International journal of environmental research and public health, 17(14), 5014. Insufficient Sun Exposure Has Become a Real Public Health Problem
Barbería-Latasa, M., Gea, A., & Martínez-González, M. A. (2022). Alcohol, Drinking Pattern, and Chronic Disease. Nutrients, 14(9), 1954. Alcohol, Drinking Pattern, and Chronic Disease
Barrett, L. F., & Simmons, W. K. (2015). Interoceptive predictions in the brain. Nature reviews. Neuroscience, 16(7), 419–429. Interoceptive predictions in the brain
Gad, I., Tan, X. C., Williams, S., Itawi, S., Dahbour, L., Rotter, Z., Mitro, G., Rusch, C., Perkins, S., & Ali, I. (2022). The Religious and Spiritual Needs of Patients in the Hospital Setting Do Not Depend on Patient Level of Religious/Spiritual Observance and Should be Initiated by Healthcare Providers. Journal of religion and health, 61(2), 1120–1138. The Religious and Spiritual Needs of Patients in the Hospital Setting Do Not Depend on Patient Level of Religious/Spiritual Observance and Should be Initiated by Healthcare Providers
Giménez, M. C., Hessels, M., van de Werken, M., de Vries, B., Beersma, D. G., & Gordijn, M. C. (2010). Effects of artificial dawn on subjective ratings of sleep inertia and dim light melatonin onset. Chronobiology international, 27(6), 1219–1241. https://doi.org/10.3109/07420528.2010.496912
Irwin M. R. (2019). Sleep and inflammation: partners in sickness and in health. Nature reviews. Immunology, 19(11), 702–715. Sleep and inflammation: partners in sickness and in health
Kang, J., Scholp, A., & Jiang, J. J. (2018). A Review of the Physiological Effects and Mechanisms of Singing. Journal of voice: official journal of the Voice Foundation, 32(4), 390–395. A Review of the Physiological Effects and Mechanisms of Singing
Puchalski, C. M., King, S. D. W., & Ferrell, B. R. (2018). Spiritual Considerations. Hematology/oncology clinics of North America, 32(3), 505–517. https://doi.org/10.1016/j.hoc.2018.01.011
Tamplin, J., Baker, F. A., Grocke, D., Brazzale, D. J., Pretto, J. J., Ruehland, W. R., Buttifant, M., Brown, D. J., & Berlowitz, D. J. (2013). Effect of singing on respiratory function, voice, and mood after quadriplegia: a randomized controlled trial. Archives of physical medicine and rehabilitation, 94(3), 426–434. Effect of Singing on Respiratory Function, Voice, and Mood After Quadriplegia: A Randomized Controlled Trial
Willemse, S., Smeets, W., van Leeuwen, E., Nielen-Rosier, T., Janssen, L., & Foudraine, N. (2020). Spiritual care in the intensive care unit: An integrative literature research. Journal of critical care, 57, 55–78. https://doi.org/10.1016/j.jcrc.2020.01.026
Zielinski, M. R., & Gibbons, A. J. (2022). Neuroinflammation, Sleep, and Circadian Rhythms. Frontiers in cellular and infection microbiology, 12, 853096. Frontiers | Neuroinflammation, Sleep, and Circadian Rhythms